Having radiotherapy to the brain (prophylactic cranial irradiation)
Radiotherapy uses radiation, usually x-rays, to destroy cancer cells.
Doctors use radiotherapy to the brain in people with small cell lung cancer who has limited disease. Radiotherapy to the brain kills any cancer cells that might have spread into the brain but are too small to see. This is also called prophylactic cranial irradiation (PCI).
When you might have prophylactic cranial irradiation
Your doctor will suggest radiotherapy to the brain if you have small cell lung cancer with limited disease, and:
- you are well enough
- your cancer has responded to chemotherapy and radiotherapy (first line treatment)
You usually have up 10 treatments.
Some people with small cell lung cancer who have extensive disease might also be offered PCI. Research shows better outcomes for people with limited disease.
The planning CT scan
Before your radiotherapy you have a planning session and a planning CT scan.
The planning session takes between 15 minutes and 2 hours.
You also have a mask (shell) made that keeps your head very still.
Radiotherapy mask (mould)
Your radiographer or technician makes your mask in the radiotherapy department. They might call the mask a radiotherapy shell.
The mask covers your face, and the top and sides of your head. It attaches to the couch when you are lying down for the planning scan or radiotherapy treatment.
The process of making the mask can vary slightly between hospitals. It usually takes around 30 minutes.
Before making the mask
You need to wear clothes that you can easily take off from your neck and chest. You also need to take off any jewellery from that area.
Facial hair, long hair or dreadlocks can make it difficult to mould the mask. Your radiotherapy team will tell you if you need to shave or tie your hair back.
Making the mask
The technician uses a special kind of plastic that they heat in warm water. This makes it soft and pliable. They put the plastic on to your face so that it moulds exactly. It feels a little like a warm flannel and is a mesh with holes in so you can breathe.
After a few minutes the mesh gets hard. The technician takes the mask off and it cools down. You might need to have one more fitting to make sure it is exactly right.
You wear the mask for your planning CT scan. Your radiotherapy team keep the mask in the department for when you go back for treatment. You wear it for each treatment session.

Voiceover: Making a mesh mask for radiotherapy takes a few minutes.
Radiographer: I am just going to heat this up now if you just keep nice and still there and just want to close your eyes for us.
Voiceover: The radiographer softens the mask by putting it in warm water for a minute or two. When the radiographer puts the mask on to your face it will feel warm and damp. They then clip it to the bed that you are lying on. It takes a minute or two to dry into the shape of your face. The radiographers will mark the mask where the light lines are.
Radiographer: Okay, you are just going to feel us pressing down on the mask there; you are doing really well are you still okay?
Patient: Mmm...
Voiceover: They use the marks on the mask to line up the machine each time you have treatment. The mask keeps you head still and makes sure that your treatment is directed at the cancer. They put your name on the mask and keep it in the radiotherapy department ready for your treatment.
Patient: They um told me about the procedure, a mask being fitted, uumm that it would be moulded to the shape of my face. Umm which they did, three lovely girls umm put my mind at ease, sat me down, heated the mask, moulded it around my face, um not an uncomfortable thing at all to go through.
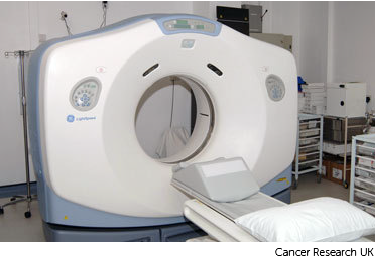
The radiotherapy room
Radiotherapy machines are very big and could make you feel nervous when you see them for the first time. The machine might be fixed in one position. Or it might rotate around your body to give treatment from different directions. The machine doesn't touch you at any point.
Before your first treatment, your  will explain what you will see and hear. In some departments, the treatment rooms have docks for you to plug in music players. So you can listen to your own music while you have treatment.
will explain what you will see and hear. In some departments, the treatment rooms have docks for you to plug in music players. So you can listen to your own music while you have treatment.

Before each treatment session
Your radiographers help you to get into position on the radiotherapy table. If you need to wear a mask for your radiotherapy, they will position the mask over your face and attach it to the table. The mask keeps your head completely still while you have treatment.
During treatment
You need to lie very still. Your radiographers might take images (x-rays or scans) before your treatment to make sure that you're in the right position. The machine makes whirring and beeping sounds. You won’t feel anything when you have the treatment.
Your radiographers can see and hear you on a CCTV screen in the next room. They can talk to you over an intercom and might ask you to hold your breath or take shallow breaths at times. You can also talk to them through the intercom or raise your hand if you need to stop or if you're uncomfortable.
You won't be radioactive
This type of radiotherapy won't make you radioactive. It's safe to be around other people, including pregnant women and children.
Travelling to radiotherapy appointments
You might have to travel a long way each day for your radiotherapy. This depends on where your nearest cancer centre is. This can make you very tired, especially if you have side effects from the treatment.
You can ask your radiographers for an appointment time to suit you. They will do their best, but some departments might be very busy. Some radiotherapy departments are open from 7 am till 9 pm.
Car parking can be difficult at hospitals. Ask the radiotherapy staff if you are able to get free parking or discounted parking. They may be able to give you tips on free places to park nearby.
Hospital transport may be available if you have no other way to get to the hospital. But it might not always be at convenient times. It is usually for people who struggle to use public transport or have any other illnesses or disabilities. You might need to arrange hospital transport yourself.
Some people are able to claim back a refund for healthcare travel costs. This is based on the type of appointment and whether you claim certain benefits. Ask the radiotherapy staff for more information about this and hospital transport.
Some hospitals have their own drivers and local charities might offer hospital transport. So do ask if any help is available in your area.
Side effects of radiotherapy to the brain
Radiotherapy to the brain can cause side effects. Let your doctor, nurse or radiographer know about any side effects that you have. Then they can find ways to help you.
Side effects usually get worse around the second week of treatment and will be at their worst at the end or just after your treatment course.
They generally last a number of weeks. Some might last for a few months after the treatment has finished.
Radiotherapy to the brain can make you feel very tired. The tiredness usually comes on gradually as you go through your treatment. By the end of the course of treatment you may feel very tired.
The tiredness usually carries on for about 6 to 8 weeks and then starts to get better.
In a few people, the tiredness can become very severe a few weeks after the end of treatment. You might also feel drowsy and irritable. This is a rare side effect and is called somnolence syndrome. It doesn't need treatment and gets better on its own over a few weeks.
It is important to rest or sleep when you need to. But it is likely to help if you can get some regular exercise. A daily walk is good if you are able to do that.
You might feel sick at times. You can have anti sickness medicines. Let your treatment team know if you still feel sick, as they can give you another type.
Tell your healthcare team if you keep getting headaches. They can give you painkillers to help.
Your skin will always be more sensitive to the sun after treatment. If you have no hair, remember to keep your head covered or wear a hat if you go outside. Or you need to wear a complete sun block.
Your skin might go red or darker in the treatment area. You might also get slight redness or darkening on the other side of your body. This is where the radiotherapy beams leave the body.
The red or darker areas can feel sore. This may start after your radiotherapy treatment is completed. Your radiographers may give you creams to soothe your skin. The soreness usually goes away within 2 to 4 weeks of ending the treatment. But your skin might always be slightly darker in that area.
Radiotherapy to the brain can cause hair loss in the treatment area. Your hair usually starts to grow back a few months after treatment ends. But this growth may be patchy at first.
Long term side-effects
There is a small chance that radiotherapy will affect your brain. Some people might have problems with memory, movement, or the ability to think or reason (cognitive function). If you are worried about this, talk to your doctor.



