Treatment for spinal cord compression
Treatment for spinal cord compression should start as soon as possible, usually within 24 hours of diagnosis. This reduces the chance of permanent damage to the spinal cord.
Treatment can also control symptoms of compression. Some people have pain. Other people have nerve symptoms, such as numbness or tingling.
Your doctor will talk to you about your options. Treatment aims to get you back to normal as much as possible and as soon as possible.
Treatment options include:
steroids 
radiotherapy 
- surgery
bisphosphonate drugs 
- other cancer treatments such as
chemotherapy  ,
, hormone therapy  or
or targeted cancer drugs 
Planning your treatment
A team of doctors, and other professionals discuss the best treatment and care for you. They are the multidisciplinary team (MDT). Your MDT might include:
- an oncologist - a doctor specialising in cancer treatment
- a haematologist - a doctor specialising in blood cancers (if you have myeloma)
- a pathologist - a doctor who diagnoses cancer from looking at cells under the microscope
- a radiologist – a doctor specialising in reading x-rays and scans
- a specialist nurse – also called a clinical nurse specialist (CNS)
- a palliative care doctor - a doctor specialising in controlling cancer symptoms
- a physiotherapist - a person trained to help you improve your movement and function
- a spinal surgeon - a surgeon specialised in treating spinal problems
When planning your treatment your doctor will consider:
- your general health and fitness
- what you are able to do
- any treatment you have already had
- the possible side effects of treatment
- the stage of your cancer
- the part of your spine affected
- your wishes and needs
Questions you can ask
Below are some questions you might want to ask your doctor about your treatment and care:
- What treatment options do I have?
- What are the risks and the benefits of each treatment option?
- What is the aim of the treatment?
- Do you think my symptoms might get worse in the future?
- What can be done to help with my pain?
- Who do I get in touch with if if my symptoms get worse, or if I develop any new symptoms?
Lying flat (bed rest)
You might need to lie flat for some time. This is to reduce movement in your spine and prevent any more damage to your spinal cord. The nurses will look after you so you can stay as still as possible. They will help you to change position safely if you do need to move.
The doctors and also  will examine you regularly. They assess your spine and look for any changes or improvements in symptoms. They will then decide what movement is safe for you and tell you what movement you can do. And what you shouldn't do.
will examine you regularly. They assess your spine and look for any changes or improvements in symptoms. They will then decide what movement is safe for you and tell you what movement you can do. And what you shouldn't do.
Once it is safe for you to move, the physiotherapist will help you sit up carefully and give you ways to move around. They might give you:
- a collar or brace to wear to protect your spine
- equipment to support you when you walk, such as a walking frame
- exercises
Steroids
Steroids are drugs that help reduce swelling and relieve pressure on the spinal cord. They are normally the first treatment you have.
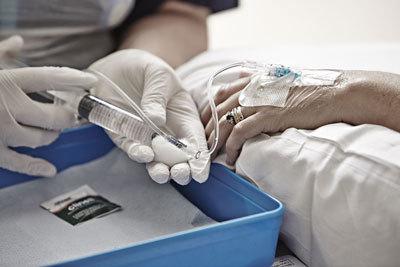
Dexamethasone is a steroid. You have it as a tablet or as a drip into your bloodstream (intravenous). You normally start having a high amount (dose). Your doctor lowers your dose as your symptoms improve. The dose reduces slowly over a few weeks if you have radiotherapy or surgery.
You take your steroids exactly as your doctor, nurse or pharmacist tells you. You should take the right dose, not more or less. Never stop taking the steroids without talking to your doctor first.
Painkillers
Pain is the main symptom of spinal cord compression. You can have painkillers to control it. You might need to try a few different types or strengths until your pain is under control.
Let your nurse or doctor know if you still have pain, for example when you move or go to the toilet. They can give you extra painkillers or ‘top-ups’ at these times.
You might have other treatments such as steroids, radiotherapy or surgery. These aim to reduce the pressure on the spinal cord and can also help to control the pain.
Your doctor might refer you to the palliative care team or symptom control doctors. They specialise in managing pain and other difficult symptoms. There are also palliative care teams in the community if you have pain when you go home.
Radiotherapy
Radiotherapy uses high energy x-rays to destroy cancer cells.. By relieving pressure on the spinal cord it can help reduce pain and improve other symptoms.
Depending on your situation you might have other treatments with radiotherapy including:
- painkillers
- steroids
- surgery
Each radiotherapy treatment is called a fraction and takes a few minutes. You might have one dose of radiotherapy to help with the pain. Or you might have a number of treatments over 5 to 10 days.
The number of fractions you need depends on your general health and other treatments you are having, such as surgery.
Your doctor will tell you how many fractions you need.
Surgery
Your doctor might suggest you have surgery to treat cancer affecting your spine. Spinal surgery is not suitable for everyone. It can be a big operation so you need to be well enough.
There are different types of operations you might have. These are to:
- remove cancer
- relieve pressure
- make your spine more stable
You might have radiotherapy after surgery.
Your doctor will explain in detail the surgery and the possible risks after surgery.
Bisphosphonates
Bisphosphonates (pronounced bis-fos-fon-ates) are a type of drug. They can help to strengthen bones and reduce the risk of bones breaking. They can help to treat some types of cancer that cause bone problems and help reduce pain.
People with myeloma or breast cancer might have bisphosphonates to help control pain and strengthen the bones in the spine. If you have prostate cancer, you might have bisphosphonates if painkillers are not working well enough.
Targeted cancer drugs
Denosumab is a type of targeted cancer drug called a monoclonal antibody. It helps strengthen the bones and reduces the risk of them breaking. You have it as an injection under the skin.
Injecting bone cement into the spine
You might have this treatment if painkillers aren’t controlling your pain. Or you might have it if the bones of the spine have collapsed.
Vertebroplasty or kyphoplasty are two ways of injecting special medical cement into the spine.
With a vertebroplasty your doctor injects the medical cement into the area where the swelling is pressing on the spinal cord.

Kyphoplasty is similar, but your doctor uses a balloon through a needle to help create the normal shape of the bone.

Chemotherapy
You might have chemotherapy for spinal cord compression. This is most likely if you have lymphoma, germ cell cancer or small cell lung cancer.
Chemotherapy uses anti cancer (cytotoxic) drugs to destroy cancer cells. Chemotherapy drugs circulate throughout your body. So it can treat cancer cells almost anywhere in the body.
Hormone therapy
Hormone therapy works by blocking or lowering the amount of hormones in the body to stop or slow down the growth of cancer. You might have hormone therapy to treat cancer that has spread to the spine. For example, if you have prostate cancer that has spread to the spine you might have the hormone therapy drug Degarelix.
Treating and preventing other problems
Having spinal cord compression means you are more likely to develop other health problems. These can happen because you aren’t able to move about as normal.
Blood clots
Lying still increases your risk of blood clots. Wearing elastic compression stockings helps to lower your risk. You might also have an anticoagulant (blood thinning) medicine. You have this as a tablet or an injection under the skin.
Chest problems
Lying down in bed can increase your risk of a chest infection. A physiotherapist can teach you deep breathing exercises. This helps to reduce your chance of getting a chest infection.
When you are ready, your nurses will help you sit up. It’s important to sit up and out in a chair if it is safe to do so. Sitting up helps you breathe more deeply and reduces your risk of infections.
Pressure sores
To prevent pressure sores you need to change position regularly. Your nurses will turn you regularly if you are on bed rest and unable to move. You will be encouraged to get out of bed and walk regularly if you are able to.
You might have a pressure relieving cushion for when you sit up.
Bladder and bowel problems
Pressure on your nerves might make it difficult for you to control your bladder or bowels. You may need a tube called a catheter to drain the bladder. You might also need medicines to help your bowel work.
Going home
Your doctors and nurses will start planning for when you go home while you are in hospital. This includes referring you for
district nursing  support
support- community
palliative care 
Physiotherapists and  should also work out a plan with you and your family. They aim to make sure you can live as independently as possible if you still have problems moving around. They can do a home visit. And then arrange equipment, such as a wheelchair, or changes to your home, such as grab rails.
should also work out a plan with you and your family. They aim to make sure you can live as independently as possible if you still have problems moving around. They can do a home visit. And then arrange equipment, such as a wheelchair, or changes to your home, such as grab rails.
Your local social services may also provide equipment or any care or help you need.
Research and clinical trials
Researchers around the world are looking at better ways to prevent, diagnose and treat spinal cord compression. These studies are looking at:
- different types and ways of giving radiotherapy
- combining radiotherapy with different drugs such as
bisphosphonates 
- using heat therapy (thermal ablation) with a type of radiotherapy called stereotactic radiotherapy (SBRT)



