Radiotherapy for acute myeloid leukaemia (AML)
Radiotherapy means the use of radiation, usually x-rays, to treat cancer. Doctors use a type of radiotherapy called external radiotherapy for acute myeloid leukaemia.
External radiotherapy uses a machine outside the body to direct radiation beams at the cancer to destroy it.
How does radiotherapy work?
Radiotherapy treatment works by damaging the  within the cancer cells. DNA is the genetic code that controls how the body's cells behave.
within the cancer cells. DNA is the genetic code that controls how the body's cells behave.
When do you have radiotherapy for acute myeloid leukaemia?
You might have radiotherapy to:
- the whole body (total body irradiation, TBI) as part of conditioning treatment for a
stem cell transplant  .
. - AML that has formed a lump outside the bone marrow (also known as myeloid sarcoma, granulocytic sarcoma, chloroma or extramedullary myeloid tumour)
- the brain or spinal cord if AML has spread there, although it is rare for this to happen
Your healthcare team will explain the type of radiotherapy treatment you will be having.
How long is a course of radiotherapy?
You might have radiotherapy as a single treatment or a series of daily treatment sessions. A single dose of radiotherapy is called a fraction. A series of sessions makes up a radiotherapy course.
The number of treatment sessions you need depends on your situation. Your doctor will discuss with you how many sessions you need.
Total body irradiation (TBI)
Conditioning treatment prepares you for a stem cell transplant. TBI is part of the conditioning treatment. The number of radiotherapy fractions you have depends on the type of conditioning you have. For example, for reduced intensity conditioning (RIC) you may have 1 or 2 fractions. With full intensity (myeloablative) conditioning you might have up to 8 treatment sessions over 4 days. So 2 fractions a day.
Planning radiotherapy for acute myeloid leukaemia
Before you begin your treatment, the radiotherapy team carefully plan your external beam radiotherapy. This means working out how much radiation you need to treat the cancer and exactly where you need it.
Your planning appointment may take from 15 minutes to 2 hours.
You usually have a planning CT scan in the radiotherapy department.
The scan shows the cancer and the area around it. You might have other types of scans or x-rays to help your treatment team plan your radiotherapy. The plan they create is just for you.
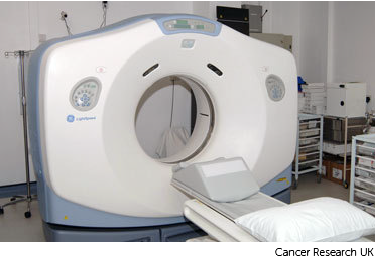
Your radiographers tell you what is going to happen. They help you into position on the scan couch.
The CT scanner couch is the same type of bed that you lie on for your treatment sessions. You have to lie as still as you can, so that the measurements are accurate and the radiographers can record your exact position. This means they can make sure you are lying in the correct position every time you have treatment.
Having the scan
Once you are in position your radiographers put some markers on your skin. They move the couch up and through the scanner. They then leave the room and the scan starts.
The scan takes about 5 minutes. You won't feel anything. Your radiographers can see and hear you from the CT control area where they operate the scanner.
Watch our video about radiotherapy planning, this is just under 3 minutes long.
Daniel (radiographer): Radiotherapy planning will involve you coming for an appointment for a CT scan in the radiotherapy department. The idea behind this is that the doctor needs to work out exactly where needs to be treated and where we need to avoid and so that scan starts us off on that process.
For the CT scan, most of the time no preparation is needed beforehand but if any is then you’ll receive that in a letter so for example, depending on what you having treated there might need to be a contrast agent introduced or you may need to have a full or an empty bladder depending on what is necessary for the scan. There are a number of things we do to help people keep still and make sure the cancer is treated.
It is important that you lie in the same position every time you have treatment. This is to make sure the radiotherapy is directed at the cancer and normal tissues are avoided. We may put equipment in place to fix your position. If you are having radiotherapy for a head and neck cancer you will have a mask made. The mask helps you to keep your head really still during treatment. We also line up the scanner and mark your skin with a felt pen where the light lines from the machine need to be aimed.
They’ll then leave the room and start the scanner and that scan lasts usually about 2 to 3 minutes. Because pen marks can rub easily the radiographer makes them permanent after your scan by tattooing very small marks on your skin.
After the scan the radiographers will give you any information that you need before starting treatment and answer any questions that you’ve got then you are free to go home.
Patient: When I came for the first meeting to plan the treatment. It was a case of having a scan and then lying, remaining on the scan machine and then the technicians took some measurements some dimensions and when they were satisfied that they had the right angles they tattooed me.
Daniel (radiographer): The next part of planning is your doctor looking at the scan and marking out on the computer where you need treatment. Once that’s been done a physicist or a dosimetrist will start to plan your treatment. And they use very powerful computers to work out exactly what dose needs to be given and from which directions it needs to come in from.
Depending on why you are having radiotherapy the radiographer might also do some extra things during the appointment. This may include:
-
making a mould or mask for radiotherapy to the brain
-
tattooing the skin
Ink and tattoo marks
The radiographers make pin point sized tattoo marks on your skin. They use these marks to line you up into the same position every day. The tattoos make sure they treat exactly the same area for all of your treatments. They may also draw marks around the tattoos with a permanent ink pen, so that they are clear to see when the lights are low.

The radiotherapy staff tell you how to look after the markings. The pen marks might start to rub off in time, but the tattoos won’t. Tell your radiographer if that happens. Don't try to redraw them yourself.
Moulds or masks
If you are having treatment to your head you may need to have a mould (shell) made to keep you perfectly still while you have treatment.

The moulds are made in the mould room or in the CT scanning room.
After your planning session
You might have to wait a few days or up to 3 weeks before you start treatment.
During this time the physicists and your radiotherapy doctor (clinical oncologist) decide the final details of your radiotherapy plan.
Then the physicists and staff called dosimetrists plan the treatment very precisely using computers.
Having radiotherapy
The radiotherapy room
Radiotherapy machines are very big and could make you feel nervous when you see them for the first time. The machine might be fixed in one position. Or it might rotate around your body to give treatment from different directions. The machine doesn't touch you at any point.
Before your first treatment, your  will explain what you will see and hear. In some departments, the treatment rooms have docks for you to plug in music players. So, you can listen to your own music while you have treatment.
will explain what you will see and hear. In some departments, the treatment rooms have docks for you to plug in music players. So, you can listen to your own music while you have treatment.

Before each treatment session
The radiographers help you to get onto the treatment couch. You usually lie on your back and might need to raise your arms over your head.
The radiographers line up the radiotherapy machine using the marks on your body. Once you are in the right position, they leave the room.
During the treatment
You need to lie very still. Your radiographers might take images (x-rays or scans) before your treatment to make sure that you're in the right position. The machine makes whirring and beeping sounds. You won’t feel anything when you have the treatment.
Your radiographers can see and hear you on a CCTV screen in the next room. They can talk to you over an intercom and might ask you to hold your breath or take shallow breaths at times. You can also talk to them through the intercom or raise your hand if you need to stop or if you're uncomfortable.
You won't be radioactive
This type of radiotherapy won't make you radioactive. It's safe to be around other people, including pregnant women and children after your treatment.
The short video below shows how you have radiotherapy. It’s just over 2 minutes long.
Daniel (radiographer): Before your treatment starts your doctor will need to work out exactly where the treatment needs to go and also which parts need to be avoided by the treatment. To have radiotherapy you lie in the same position as you did for your planning scans. We then line up the machine based on your tattoo marks. It is really important that you stay very, very still when you are having treatment. It is also important to let the radiographers know right at the beginning if you are not comfortable so they can adjust your position.
Radiographer: Okay all done, we’ll be back in a couple of minutes.
Daniel (radiographer): We leave the room and control the room from a separate room. This is so we aren’t exposed to radiation. Treatment takes a few minutes and you will be able to talk to us using an intercom. We can see and hear you while you are having your treatment and will check that you are okay. When your treatment starts you won’t feel anything; you may hear the machine as it moves around you giving the treatment from different angles. Because we are aiming to give the same treatment to the same part of the body everyday then the treatment process is exactly the same everyday, so you shouldn’t notice any difference. You’ll see someone from the team caring for you once a week while you are having treatment. They’ll ask how you are and about any side effects.
Patient: They get you from one sitting area to another. And then take you into the room where you undress to the waist, and then lie down, and line you up by either moving you or asking you to shuffle a little. And they check the dimensions and they talk to one another and they say I am fine this side how are you ...yes fine...okay, stay where you are Jeff and that was it. There were a few little clicks and lights go on and off and you can see a green laser beam which lines up with certain things on your body uh so no, no real noise and no discomfort.
Side effects of radiotherapy
Radiotherapy for AML can cause side effects. These will depend on:
-
where you are having treatment to
-
how much radiotherapy you have (the number or fractions and overall dose)
-
if you have it with other treatments such as chemotherapy
Your healthcare team will explain possible side effects and what to do if you have them.



