Planning radiotherapy for pleural mesothelioma
The radiotherapy team plan your external radiotherapy before you start treatment. This means working out the dose of radiotherapy you need and exactly where you need it.
Your planning appointment takes from 15 minutes to 2 hours.
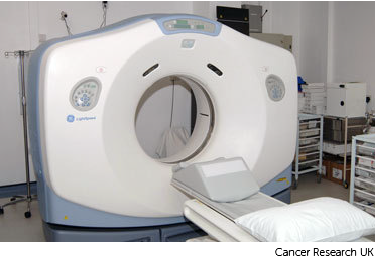
You usually have a planning CT scan in the radiotherapy department.
The scan shows the cancer and the area around it. You might have other types of scans or x-rays to help your treatment team plan your radiotherapy. The plan they create is just for you.
Your radiographers tell you what is going to happen. They help you into position on the scan couch. You might have a type of firm cushion called a vacbag to help you keep still.
The CT scanner couch is the same type of bed that you lie on for your treatment sessions. You need to lie very still. Tell your radiographers if you aren't comfortable.
Injection of dye
You might need an injection of contrast into a vein in your hand. This is a dye that helps body tissues show up more clearly on the scan.
Before you have the contrast, your radiographer asks you about any medical conditions or allergies. Some people are allergic to the contrast.
Having the scan
Once you are in position your radiographers put some markers on your skin. They move the couch up and through the scanner. They then leave the room and the scan starts.
The scan takes about 5 minutes. You won't feel anything. Your radiographers can see and hear you from the CT control area where they operate the scanner.
Ink and tattoo marks
The radiographers make pin point sized tattoo marks on your skin. They use these marks to line you up into the same position every day. The tattoos make sure they treat exactly the same area for all of your treatments. They may also draw marks around the tattoos with a permanent ink pen, so that they are clear to see when the lights are low.

The radiotherapy staff tell you how to look after the markings. The pen marks might start to rub off in time, but the tattoos won’t. Tell your radiographer if that happens. Don't try to redraw them yourself.
After the scan
The radiographers will then help you off the CT scanner couch and you can get changed back into your clothes. You stay in the department for about 15 to 30 minutes if you had an injection of the dye. This is in case it makes you feel unwell, which is rare.
You should be able to go home or back to work. You can eat and drink normally.
Possible risks
A CT scan is safe for most people but there are some possible risks. Your doctor and radiographer make sure the benefits of having the scan outweigh these risks.
Allergic reaction
Rarely, people have an allergic reaction to the contrast medium. This most often starts with weakness, sweating and difficulty breathing. Tell your radiographer immediately if you feel unwell so they can give you medicine.
Swelling around injection site
There is a risk that the contrast medium will leak outside the vein. This can cause swelling and pain in your arm but it’s rare.
Radiation
Exposure to radiation during a CT scan can slightly increase your risk of developing cancer in the future. Talk to your doctor if this worries you.
Pregnancy
Pregnant women should only have CT scans in emergencies. Contact the department as soon as you can before the scan if you are pregnant or think that you might be.
After your planning session
You might have to wait a few days or up to 3 weeks before you start treatment.
During this time the physicists and your radiotherapy doctor (clinical oncologist) decide the final details of your radiotherapy plan. They make sure that the area of the cancer will receive a high dose and nearby areas receive a low dose. This reduces the side effects you might get during and after treatment.



