Planning radiotherapy for bladder cancer
The radiotherapy team plan your external radiotherapy before you start treatment. This means working out the dose of radiotherapy you need and exactly where you need it.
Your planning appointment takes from 15 minutes to 2 hours.
You usually have a planning CT scan in the radiotherapy department.
The scan shows the cancer and the area around it. You might have other types of scans or x-rays to help your treatment team plan your radiotherapy. The plan they create is just for you.
What happens
When you arrive
The radiographer might ask you to change into a hospital gown. You should remove any jewellery and other metal objects, such as hair clips around the area being scanned. Metal interferes with the images produced by the scanner.
You might need to empty your bladder before you have the CT scan. Usually, before each radiotherapy treatment, you’ll have to empty your bladder and bowel. The radiographers go through this with you.
In the scanning room
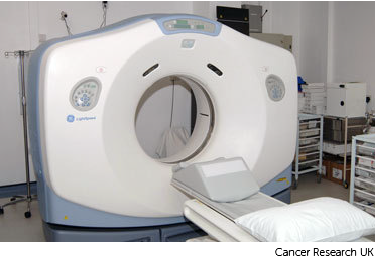
When you’re ready, the radiographer or assistant takes you into the scanning room. A CT scanning machine is large and shaped like a doughnut.
You might have an injection of contrast medium through a small tube (cannula) in your arm. You may:
- feel hot and flushed for a minute or two
- have a metallic taste in your mouth
- feel like you’re passing urine but you aren’t – this feeling is common and passes quickly
Tell the radiographer if you know you are allergic to the contrast medium.
Tell the radiographer if you feel anxious or claustrophobic about having a scan.
Having the CT scan
You usually lie down on the machine couch on your back. Once you’re in the right position, the radiographer leaves the room to protect them from the radiation. They can see you on a TV screen or through a window from the control room. You can talk to each other through an intercom.
The couch slowly slides backwards and forwards through the hole of the scanner. The machine takes pictures as you move through it.
The scan is painless but can be uncomfortable because you have to stay still. Tell your radiographers if you’re getting stiff and need to move.
During the scan
You’ll hear a whirring noise from the scanner.
The radiographer might ask you to hold your breath at times.
When the scan is over
At the end of the scan, your radiographer will mark your skin with very small dots. These permanent marks help the radiographers line you up in the same way every day for treatment. The tattoos make sure they treat exactly the same area for all of your treatments.
They make the small dots using a small needle and some dye. These marks are permanent. Your radiographer might also draw marks around the tattoo dots with a permanent ink pen. This is so they are clear to see when they are lining you up for treatment as the lights are usually low.

Once finished the radiographer lowers the couch so you can get up.
After your planning session
You might have to wait a few days or up to 3 weeks before you start treatment.
During this time the physicists and your radiotherapy doctor (clinical oncologist) decide the final details of your radiotherapy plan. They make sure that the area of the cancer will receive a high dose and nearby areas receive a low dose. This reduces the side effects you might get during and after treatment.



